Brain hematomas occur when blood vessels in or around the brain rupture, leading to dangerous pressure buildup. Symptoms include severe headaches, nausea, confusion, and vision changes. Diagnosis typically involves CT or MRI scans, and treatment depends on severity. Acute cases often require emergency craniotomy surgery, while chronic hematomas may be treated with less invasive burr hole drainage. Recovery varies but may include physical, speech, and occupational therapy. Georgia Neurosurgical Institute offers expert treatment to ensure the best possible outcomes for patients.
Brain hematomas, in all of their various forms, are dangerous conditions in which a tear or rupture of a blood vessel causes blood to pool in or on the brain. This pooling blood puts excessive pressure on the brain, which can cause a wide range of symptoms, permanent damage to the brain, or even death.
The most severe brain hematomas can progress quickly, and time is of the essence for diagnosing and treating the injury. When a patient’s life is on the line, how is a brain hematoma detected and treated?
This month, our neurosurgical experts answer this and other questions about brain hematomas.
What Is a Brain Hematoma?
When they occur elsewhere on the body, hematomas are usually completely benign—the most common type is the everyday bruise. However, when they occur in the head, they are anything but benign and can quickly become life-threatening.
A brain hematoma occurs when a blood vessel in or around the brain becomes damaged, usually because of a traumatic injury. The damage to the blood vessel releases blood that, having nowhere else to go, collects at or near the site of the injury. Brain hematomas generally fall into one of three categories:
- Subdural hematomas occur when the blood pool is located between the dura mater and the arachnoid mater, two layers of the meninges – the membranes that lie between the surface of the brain and the skull.
- Epidural hematomas occur when blood pools between the dura mater and the skull.
- Intracranial hematomas occur when the vessel damage and subsequent blood pooling are located within the brain itself.
All three conditions cause a gamut of symptoms, including severe headaches, nausea, slurred speech, weakness, blown pupils (one pupil bigger than the other and unresponsive to light), confusion, and dizziness.
They can also vary in severity—from acute, the most severe and rapidly developing cases, to chronic, which are slower to develop and can go hidden for weeks or months before showing symptoms.
How Is a Brain Hematoma Detected?
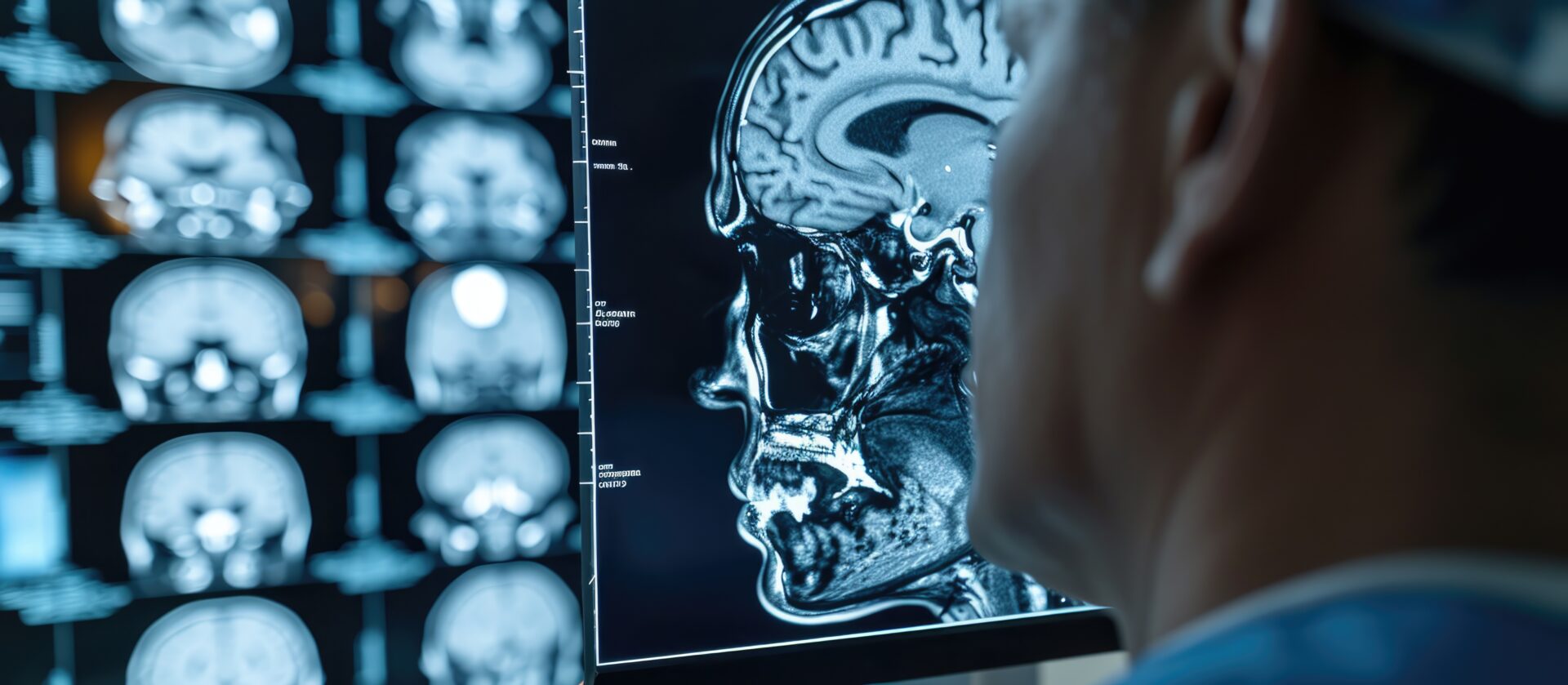
Like most medical conditions, the first stage of diagnosing a brain hematoma is observation of the patient and their symptoms. Medical professionals understand the likelihood of a hematoma developing following any traumatic head injury and will closely monitor head patients for any signs of the symptoms of hematomas. If a patient begins showing or complaining of the recognized symptoms, they will immediately be referred to diagnostic imaging for a more in-depth diagnosis. This imaging will usually take one of two forms:
- A computed tomography (CT) scan uses precision X-rays and computer modeling to create a detailed image of the injury site and show exactly where the blood is pooling.
- A magnetic resonance imaging (MRI) machine uses high-powered magnets and the property of molecular resonance to create an incredibly detailed image of the brain and hematoma.
In either case, the medical team will be able to see the hematoma and determine whether the condition is acute, chronic, or somewhere in between. If the hematoma is acute, the patient will usually be referred directly to surgery for treatment.
How Is an Acute Brain Hematoma Treated?
If a patient is suffering from an acute brain hematoma, they will usually require immediate surgical intervention to remove the excess blood and reduce the pressure on the brain. At the same time, the surgeons will find and stop the source of the bleeding to prevent further development of the hematoma.
Because of the immediate threat to life posed by an acute brain hematoma, the usual surgical response is a craniotomy. During a craniotomy, the surgical team will remove a section of the patient’s skull to allow the excess blood to drain quickly.
If the hematoma is subdural or epidural, the surgeon usually will not have to penetrate the matter of the brain itself. If the patient is suffering an intracranial hematoma, the surgical team will have to use one of a number of potential methods to enter the brain and drain away the pooling blood.
How Is a Chronic Brain Hematoma Treated?
While still dangerous, chronic brain hematomas develop much more slowly, and a less invasive surgical treatment may be an option. If a hematoma is growing slowly enough, the surgeon may elect to treat the condition with burr holes instead of a full craniotomy.
In a burr hole procedure, instead of removing a section of the skull, the surgeon drills small holes in the skull, and inserts drains that remove the pooled blood and relieve the pressure on the brain.
What Does Recovery From Brain Hematoma Treatment Look Like?
All brain hematomas are serious conditions, and recovery from one can take a considerable period. Even with the fastest possible reactions and immediate treatment, the likelihood of some level of damage to the brain is very high. Patients can wake up from a craniotomy or burr hole procedure with speech, movement, memory, cognition, or other impairments.
In many cases, these impairments will mostly resolve themselves over the course of about six months, with minor, gradual improvements continuing for a year or two after. In others, however, the damage is permanent, and a complete recovery may be impossible.
The main thing for patients to keep in mind when recovering from a brain hematoma is patience. Recovery from brain injuries is never a fast process and is usually frustrating since things that were easy to do just a few days ago may now seem almost impossible.
Patients may require a number of different follow-up therapies to address functional issues arising from the hematoma, including:
- Physical therapy to restore lost mobility
- Occupational therapy to recover the ability to perform daily functions
- Speech therapy to overcome any speech impairments
- Behavioral or emotional therapy to deal with the heavy emotional impacts of experiencing loss of function
While no patient is ever guaranteed a full recovery from a brain hematoma, patients who are able to get immediate medical attention, receive quick and effective treatment, and follow through with any prescribed therapy after treatment stand the best chance of experiencing the best outcomes.
Brain hematomas are serious events that Georgia Neurosurgical Institute is prepared to treat.
The neurosurgeons and team at Georgia Neurosurgical Institute are highly trained and experienced in treating hematomas on the brain with careful precision. The brain is the most important organ in the body—when something happens to risk its function, our team is here to treat the problem swiftly and skillfully. Your head is in good hands when you turn to our practice.
Schedule a consultation with Georgia Neurosurgical Institute today: 478-743-7092
Georgia Neurosurgical Institute offers exceptional treatments for the brain and spine to patients throughout Middle Georgia. With offices in Macon and satellite locations in Dublin, Locust Grove, and Warner Robins, we’re able to treat patients in and around:
- Dublin
- Forsyth
- Locust Grove
- Macon
- McDonough
- Milledgeville
- Perry
- Warner Robins
Related Articles







